Canine Megaesophagus – why is this happening to my dog?
Definition of Megaesophagus (simplified):
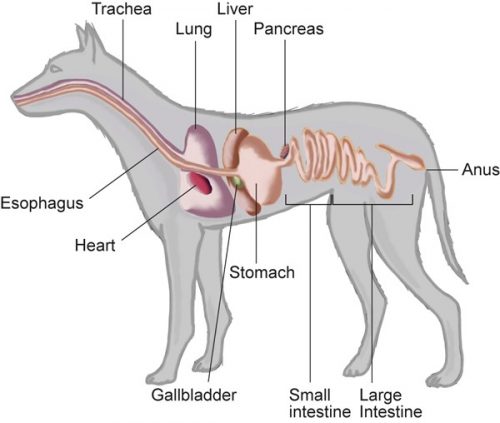
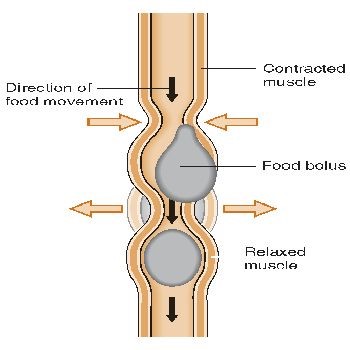
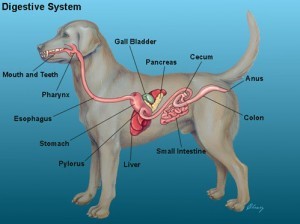
Megaesophagus is a generalized enlargement of the esophagus — a muscular tube connecting the throat to the stomach — with a decreased to absent motility. Esophageal motility is required for moving food and liquid down to the stomach.The esophagus is the tube which connects the mouth to the stomach. With megaesophagus, the esophagus is enlarged (dilated) and there is a decrease in peristalsis. Peristalsis is the wave like contractions that moves the food from the esophagus to the stomach. ME dogs have a dilated esophagus due to lack of muscle tone. This causes food to sit in the esophagus, unable to travel to the stomach and sometimes forming pockets. When this happens a dog “regurgitates” the food that is stuck in the esophagus. The dog will open his mouth and food will simply roll out. It is generally a quiet and effortless motion opposed to vomiting. Vomiting is an active motion associated with retching and heaving digested food.
Canine Digestive System Example of Peristalsis
Megaesophagus may be congenital (born with it) or acquired. Acquired ME can be further divided into two subclasses, idiopathic (cause unknown) or it can be secondary to another disease. Unless your dog is born with ME, it is very important to look at what could have caused the ME. ME is secondary to many diseases, diseases that can be treated. Many times the symptom of Megaesophagus can resolve once the proper drugs are in place. Let’s take a look…
Congenital (Idiopathic) Megaesophagus:
The majority of cases of canine megaesophagus have no apparent cause, and are therefore given the name, idiopathic megaesophagus. Congenital megaesophagus is a hereditary form of the disease that occurs in puppies. It is caused by a developmental disorder involving the nerve plexus in the lower esophagus. Peristaltic activity stops at the level where the esophagus is paralyzed, and food can go no further. Puppies with congenital ME usually show signs when they are being weaned from their mother’s milk. While milk can slide down easily, solid food tends to bulk up and the puppy will regurgitate their food. Sometimes it is noticeable right from the start. Breeders often refer to these puppies as “milk nose”. They are often the runt of the litter. It is largely the result of “esophageal hypomotility” (decrease or absence of movement or peristalsis). Sometimes esophageal hypomotility is due to delayed maturity of the esophageal function that may or may not improve with age. This is why it is so important to diagnose and start treatment early in order to prevent pockets from forming and further dilation of the esophagus. Thoracic radiography (xray) is the common diagnostic tool to determine megaesophagus.
INTERESTING NOTE: We are seeing higher rates of success with puppies born with ME having good chance to resolve the ME if: 1) They are diagnosed very early, 2) diagnosis shows just ME, and 3) if they are managed properly beginning immediately so pockets and pouches cannot form. As they grow the esophagus (which is a muscle) will strengthen and have good chance they out grow this. Best example to demonstrate this is 2 years ago we had 4 breeders find our rehoming ME dogs effort. Each had a full litter diagnosed very early with ME for a total of 42 puppies. Unbelievably, each of those breeders managed their litters using proper ME protocol, then as they began to outgrow their condition, they 1) found great homes nearby, 2) made sure the new homes had all ME info but also by contract they were required to show each was altered when of age, and 3) they had the parents altered. This was an incredible situation resulting in 40 of the 42 puppies resolving or going into complete remission from the ME. We did 1) highly recommend they always eat from a bowl placed higher (such as a chair or raised feeder) and 2) they had all our contact info to pass forward to all new homes so everyone had access to whatever support might be needed in the future.
Acquired Megaesophagus:
This type of ME is secondary to underlying disease, namely hypothyroidism or myasthenia gravis, and are thus called acquired secondary megaesophagus. Secondary acquired megaesophagus can be brought on by any disease that interferes with the esophageal peristalsis (movement) by disrupting central, efferent, or afferent nerve pathways or by any disease of the esophagus muscle system, including immune-mediated, infectious, and preneoplastic (pre stages of a tumor) causes. The wide spread causes of acquired ME can be the result of a variety of neuromuscular, immune-mediated, endocrine, gastrointestinal, paraneoplastic, and toxic diseases.
Idiopathic :
An idiopathic (cause unknown) diagnosis is made when all possible scenarios have been eliminated and all testing is complete. This can be the hardest diagnosis to accept. There is no magic pill to make it go away. Your dogs megaesophagus may stay about the same, may improve, may get worse or your dogs ME could go into remission. ME is not a death sentence. Because your veterinarian may not have seen enough cases of it to be able to make suggestions to help your dog thrive you might need to seek out a different veterinarian willing to help you become educated by using proper protocols so your dog live best quality of life.
Persistent Right Aortic Arch (PRAA) is a Vascular Ring Anomaly or (VRA):
Persistent right aortic arch is a congenital abnormality of the blood vessels of the heart that can affect esophageal function in some dogs and less commonly, in cats. Basically, an embryonic branch of the aorta fails to regress and is wrapped around the esophagus when a puppy or kitten is born. This puts pressure on the tube, preventing the passage of food in the esophagus when the pet eats, causing regurgitation. Surgery can correct the problem, and follow-up care can usually reverse the esophageal effects, especially if done early in a pet’s life. This vascular condition known as persistent right aortic arch is also called vascular ring anomaly (VRA) or vascular compression of the esophagus. It’s a condition that results from the abnormal development of the artery that arises directly from the heart, the aorta. More easily said, VRA is a birth defect that happens when blood vessels, known as aortic arches in the heart, fail to deteriorate as the embryo grows. The right aortic arch passes near the esophagus. If this blood vessel does not dissipate in the newborn, the esophagus is trapped between it and the heart. Food is restricted from passing by this stricture (narrowing), causing regurgitation.
While a VRA doesn’t cause a problem to the cardiovascular system itself (i.e., blood flows without impediment), the constriction of vital structures like the esophagus (the tube that carries food into the stomach) and occasionally the trachea (windpipe) can be devastating to the affected pup. The consequence of this abnormal ring around the body’s feeding tube is often regurgitation due to a compressed esophagus. Aspiration pneumonia can also result when dogs inhale the food they’re meant to ingest. Surgery is recommended to correct this condition. It should be performed as early as possible to prevent further damage to the esophagus. Many puppies born with PRAA do not have true megaesophagus. Once the stricture is removed these puppies can eat normally in the majority of cases. A barium contrast esophagram (barium swallow) can confirm the presence of PRAA (Persistent Right Aortic Arch).
SPECIAL NOTE: As said in the above Interesting Note, same holds true with diagnosis of PRAA/VRA. Biggest difference is consistency of the food must be very thin liquid so it can pass thru the strictured area. It is also important to get the surgery performed as early as possible but between diagnosis and the surgery, they must be upright for anything taken in so 1) food has best chance to pass to stomach and 2) they can be stable enough to survive this surgery. In a few cases, the puppies have had a temporary feeding tube placed so they can bypass the strictured area. But they must still be fed upright and stay long enough for food to pass. After surgery, the feeding tube should be able to be removed at surgeons discretion.
SPECIAL WARNING: IF you are getting this surgery done, do your homework and make sure all bases are covered from diagnosis to release of puppy from surgeons care. ASK for whatever information you need, become highly educated to what happens and when, AND make sure you feel comfortable the surgeon you choose WILL follow though safely afterwards by closely monitoring your dog. Sadly, from experience, there are always great surgeons out there to perform this surgery successfully. However, it is just as critical to have proper care beginning immediately after surgery has ended. The puppy MUST still be elevated during recovery, then when they can begin to try food, in whatever manner the surgeon wishes, again they MUST be upright then held that way for gravity to take the food down. We have known several puppies who died not from the surgery, but gross human errors shortly afterwards. One was due to the person transporting the puppy back home. They were under strict guidelines from the excellent surgeon, but during the drive home felt “sorry” because the puppy seemed hungry so gave it a chicken nugget. Sadly, this precious puppy choked and died shortly after. Then others were at very experienced, well known locations well versed with the right surgeons, BUT not in monitoring care afterwards. The persons responsible flor feeding and monitoring afterwards did not follow proper protocol and these puppies died needlessly.
Congenital Myasthenia Gravis:
Myasthenia Gravis in dogs is an autoimmune disease that impacts the neuromuscular junction in canines, cats, and humans. It is caused by a breakdown of acetylcholine (ACh) receptors, which are basically linked to the transmission of impulses from nerves to the muscles. This condition causes severe muscle weakness throughout the body. Congenital MG is an inherited autosomal recessive condition (meaning two copies of an abnormal gene must be present in order for the disease or trait to develop). It is found in Parson Russell Terriers, Springer Spaniels, and Smooth Fox Terriers. They are born without the acetylcholine receptors (AChRs) at the neuromuscular junction. Puppies that are born with Congenital MG present similar to acquired MG with general muscle weakness to the striated skeleton muscles and megaesophagus. Measurement of acetylcholine receptor antibody titer is not a diagnostic tool for congenital MG. A muscle biopsy is needed to diagnose this condition. The outcome for Congenital Myasthenia Gravis is not good since traditional treatment for MG is not effective.
Congenital Myasthenia Gravis is incredibly rare, but it can happen. Puppies born with an ACh-receptor (acetylcholine receptors) deficiency are likely to have congenital Myasthenia Gravis. Congenital Myasthenia Gravis typically becomes apparent in puppies that are approximately six to eight weeks old. In severe cases of Congenital Myasthenia Gravis, puppies can experience paralysis or even death. See the Chapter on Myasthenia Gravis (MG) for detailed information.
Acquired Myasthenia Gravis:
Myasthenia Gravis in dogs is an autoimmune disease that impacts the neuromuscular junction in canines, cats, and humans. It is caused by a breakdown of acetylcholine (ACh) receptors, which are basically linked to the transmission of impulses from nerves to the muscles. This condition causes severe muscle weakness throughout the body. This disease is said to be the cause of 25% or more of Canine Megaesophagus. Early diagnosis and treatment is the key to success with this disease. Since 90% of dogs with MG have ME also as a symptom, controlling the ME is most important. Aspiration Pneumonia continues to be the biggest threat here. Important to remember: Dogs with MG can go into remission on average in 6-8 months and sometimes their ME can resolve as well. ALL DOGS THAT ARE NOT BORN WITH ME AND ARE DIAGNOSED WITH ME SHOULD BE TESTED FOR MG. ALL DOGS THAT ARE DIAGNOSED WITH MG SHOULD BE TESTED FOR ME! See the Chapter on Myasthenia Gravis (MG) for detailed information.
Acquired Myasthenia Gravis typically appears in dogs that are between two and four years old. Acquired Myasthenia Gravis in dogs is an immune-mediated disease, which is when the dog’s own antibodies destroy ACh-receptors, causing an acetylcholine receptors deficiency.
Possible Neuromuscular and Immune-Mediated causes include:
• Botulism
• Canine Distemper
• Dermatomyositis
• Dysautonomia
• Glycogen storage disease (GSD)
• Laryngeal paralysis-polyneuropathy complex (LP-PNC)
• Myasthenia Gravis
• Neosporosis
• Polymyositis
• Polyneuropathy
• Tetanus
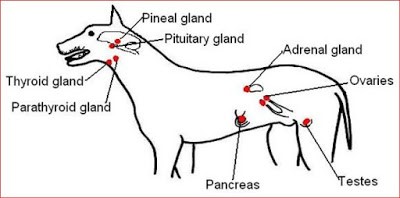
Endocrine Causes:
The endocrine system is composed of several different types of glands and organs that produce the hormones of the dog’s body. A hormone is a chemical that is secreted by a gland in one area of the body and is carried by the bloodstream to other organs in the body, where it exerts some effect. Most hormones regulate the activity or structure of their target organs. The overall effect of the endocrine system is to regulate, coordinate and control many different bodily functions. The endocrine system includes the hypothalamus, pituitary gland, thyroid gland, parathyroid glands, adrenal glands, part of the gastrointestinal tract, pancreas, kidneys, liver, ovaries and testes. Addison’s Disease (Hypoadrenocorticism) and Hypothyroidism are the two most common endocrine causes. Both can be reversible so warrants evaluation and discussion with your veterinarian.
Addisons Disease:
Dogs with Addison’s disease may have megaesophagus due to electrolyte imbalances and a cortisol deficiency. Electrolyte imbalances cause altered membrane potentials, which result in decreased neuromuscular functions. Muscle weakness is a symptom of deficient cortisol. Addison’s Disease is the common name for hypoadrenocorticism, or adrenal insufficiency. There are three forms of Addison’s disease:
– Primary
– Secondary
– Atypical
Primary and atypical Addison’s are usually the result of immune mediated damage to the glands. Secondary hypoadrenocorticism is from failure of the pituitary to stimulate the adrenals with adrenocorticotropic hormone (ACTH). It is important for you to know which type of Addison’s disease your dog is being treated for. Symptoms of Addison disease may include weakness, depression, loss of appetite, vomiting, diarrhea, and sometimes increased thirst and urination and Megaesophagus. The confirming test for Addison’s disease is an ACTH stimulation test. In this test, blood samples are taken before and after the dog is injected with an adrenal-stimulating hormone. If your dog has primary Addison’s, which means both layers of the adrenal gland are under-producing hormones, fludrocortisone is usually prescribed. There is also an injectable drug called DOCP, brand name Percorten V. This is a long-acting drug given by injection every 25 days. The drug is given primarily to regulate electrolytes, so cortisol replacement will also be needed. This means both an injection and an oral daily cortisone drug. For dogs with atypical or secondary Addison’s, only glucocorticoid replacement (Prednisone, for example) is given.
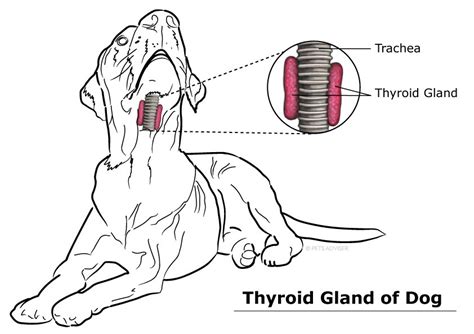
Hypothyroidism:
The thyroid gland is in the neck. It makes a hormone called thyroxine that controls metabolism (the process of turning food into fuel). With hypothyroidism, the gland doesn’t make enough of that hormone. It’s a common disease in dogs. It affects all breeds, but it is often found in Golden Retrievers, Doberman Pinschers, Irish Setters, Dachshunds, Boxers, and Cocker Spaniels. It usually happens in middle-aged dogs (ages 4 to 10) of medium to large breeds. Neutered males and spayed females also have a higher risk, but vets are unsure why. It is thought that in some cases of hypothyroidism, your dog’s immune system attacks his thyroid. Other causes are the shrinking of his thyroid and, although rare, a tumor of the thyroid gland. No matter the cause, symptoms and treatments are the same.This is a disease of thyroid deficiency. Dogs with Hypothyroidism have metabolic rates below normal. The most common symptom is hair loss that involves the front of the neck down to the chest, the sides of the body, the backs of the thighs, and the top of the tail. The hair is excessively dry and brittle, and falls out easily. The exposed skin is dry, thick, puffy, and darkly pigmented. Some dogs develop secondary seborrhea. Other signs include weight gain, intolerance to cold, slow heart rate, absence of heat cycle, lethargy, corneal ulcers, deafness and Megaesophagus. It is easy to test for and easy to treat. Your vet will take a simple blood test to check the levels of T3 and T4. If this blood test is low it is a red flag for hypothyroidism. It is effectively treated with a daily or twice a day thyroid hormone replacement using synthetic L-thyroxine (L-T4)(Levathyroxine). Many times once the thyroid is well regulated the ME resolves as well. Megaesophagus occurs in 3% of hypothyroid dogs.
Gastrointestinal Causes:
Gastrointestinal disorders associated with acquired megaesophagus:
Esophagitis:
Esophagitis can lead to Megaesophagus if not treated properly. Acid reflux is the most common cause of esophagitis. Acid reflux is the result of stomach acids passing into the esophageal canal, causing irritation to the tissue lining of the esophagus. Intubation for anesthesia for surgery can also cause esophagitis. Chronic vomiting, dog swallowed a foreign body, retaining ingested pills or capsules, infections and accidental ingestion of irritant chemicals can also cause esophagitis. Megaesophagus comes into play if the condition has progressed to the point that the esophagus has formed a stricture (narrowing) or a pocket where food will lodge itself and the dog regurgitates. Endoscopy (a long thin tube with a tiny camera on the end) may be recommended as a diagnostic tool to differential between esophagitis and megaesophagus or to rule out an obstructive lesion or a tumor. Carafate/Sucrafate to sooth the esophagus is usually prescribed plus a pain reliever such as Tramadol.
Esophageal obstruction:
Esophageal obstruction can be caused by esophageal foreign bodies, neoplasia (tumors), strictures (narrowing of the esophagus sometimes caused by scar tissue), or vascular ring anomalies. Foreign bodies or chronic gastroesophageal reflux (GERD) can cause esophageal strictures (scar tissue). The buildup of gastric stomach acid (pepsin and bile salts) and other components of the gastrointestinal juices can cause damage to the protective mucus lining of the esophagus. This can lead to esophagitis (inflammation of the esophagus) and later lead to scar tissue forming in the esophagus. An antacid is often times prescribed to reduce acid reflux. Esophageal obstruction can also be caused by vascular ring anomalies. In 95% of the cases secondary megaesophagus is caused by PRAA (Persistent Right Aortic Arch) Other vascular anomalies associated with secondary megaesophagus included persistent right or left subclavian arteries, double aortic arch, persistent right dorsal aorta, left aortic arch, right ligamentum arteriosum, aberrant intercostals arteries, and persistent left cranial vena cava.
Gastric Dilatation Volvulus (GDV):
Dog with chronic “bloat” (GDV) with or without volvulus (the stomach rotates or twist in the abdomen), have an increase risk of developing megaesophagus. In these dogs, megesophagus is due to a weak lower esophageal sphincter (LES) caused by a combination of esophagitis from chronic GERD or vomiting; chronic intermittent obstruction of the LES; increased intragastric and intraabdominal pressures; and delayed gastric emptying. Promotility drugs that may be effective in emptying the stomach are Metroclopramide (Reglan) and Cisapride. Bloat occurs when the dog’s stomach fills with gas and twists, cutting off blood and oxygen to the stomach. As the swollen stomach pushes against surrounding organs and large blood vessels, blood flow to the heart eventually stops. Without immediate treatment, shock and a painful death occurs within minutes. Any dog can have GDV, larger deep chested dogs are more at risk. It is suggested that you avoid strenuous exercise after eating or drinking, eating slower and more frequent meals may help as well. Dogs with chronic GDV may need a surgery called “gastropexy”. This surgery returns the stomach to the normal position permanently by surgically attaching the stomach to the abdominal wall to prevent twisting.
Hiatal Hernia:
Any time an internal body part pushes into an area where it does not belong, it’s called a hernia. In the case of a hiatal hernia the esophagus is essentially obstructed. There are two types of hernias that canines can have, a Type 1 or “sliding” hernia or Type II a paraesophageal or “rolling” hernia. Xrays and CT imaging are used as diagnostic tools. Fluoroscopy, which is a real-time radiographic procedure that utilizes a low dose, continual x-ray transmitted through the body onto a fluorescent screen and generates a short dynamic movie-like study, may show motility in motion. Temporary relief of symptoms may be achieved with drugs such as omeprazole (Prilosec) and cimetidine (Tagamet). In most cases surgery to correct the hernia is required, usually involving surgical reduction of the hernia followed by placation of the esophagus hiatus and left flank gastropexy.
Thymoma Causes:
Thymomas (paraneoplastic) are tumors or masses which can be either benign (non-invasive) or malignant (invasive) and are found in older dogs, with the mean age being approximately 9 years old. While there has been no particular breed predisposition for thymoma development, it seems that medium and large sized dogs are afflicted more often than smaller breeds. The thymus gland, in which the tumor develops, is located in the chest cavity, just in front of the heart. The close proximity of the thymus gland to the heart and lungs makes a malignancy especially serious. Thymomas are defined as rare tumors which grow in the lining (epithelium) of the thymus gland of both dogs and cats, usually being found in older animals. Megaesophagus is present in 40% of dogs with a thymoma. A thymoma is a tumor of the thymus organ. The thymus is located in front of the heart in the rib cage. It is part of the lymphatic system. It produces lymphocytes (white blood cells) called T-cells. These white blood cells are important because they kill foreign cells, and activate other immune cells to fight infection. They also stop the immune response after a foreign cell has been eliminated. T-cells migrate away from the thymus to other parts of the body such as the lymph nodes, spleen and the bloodstream. As the pet matures, the thymus has served it function and it will wither away. The incidence of a thymoma in dogs with MG is about 3%. The prognosis of a dog with MG with a thymoma is poor. However, removing the tumor can result in resolution of Megaesophagus and a decreased AChR antibody titer.
NOTE: Paraneoplastic syndromes may be seen in any dog with a malignant (most common) or benign tumor (rare). Paraneoplastic syndromes (PNS) are a group of disorders that result from the abnormal secretions of a hormone or hormone-like product from a cancerous tumor, or from the body’s immune response to the tumor.
Toxic Causes:
Lead:
Low-level lead exposure causes severe abdominal pain, vomiting, diarrhea and megaesophagus. Lead intoxication can occur from ingestion of batteries, fishing line weights, lead-based pain, linoleum, and plumbing or solder supplies. A serium blood test to confirm toxicity is available commercially.
Organophosphates:
Organophosphate toxicosis should be suspected if a dog presents with concurrent weakness and cerebellar signs. Organophosphates exist in flea collars and insecticides. Organophosphate toxicity may lead to chronic anorexia, muscle weakness and muscle twitching which may last for days or even weeks. Organophosphate insecticides inhibit cholinesterases and acetylcholinesterase, essential enzymes in the body. Cholinesterases are enzymes which break down acetylcholine, which is a neurotransmitter. Consequently, acetylcholine remains attached to the postsynaptic receptors of the neurons causing continuous, unending nervous transmission to nervous tissue, organs and muscles (smooth and skeletal). This causes seizures and shaking. A blood test to confirm toxicity is available.
Snake Venom:
Australian Tiger Snake venom causes a rapidly progressing myopathy (disease resulting in muscle weakness) of skeletal muscle. If not lethal, Australian Tiger snake venom has a 75% recovery rate for normal esophageal function. This snake is found in southern regions of Australia, including its coastal islands of Tasmania.
Incidental or Temporary ME:
Incidental esophageal dilation is associated with excitement, aerophagia (intestinal gas) general anesthesia and vomiting. In cases of anesthesia and esophagitis associated megaesophagus, it should resolve within 2 to 14 days.
Medications:
Please make sure to check the medications you are giving your dog. For example Potassium Bromide, used to control seizure disorders, carries a risk of megaesophagus.